Macular Degeneration eBook
£7.81 Original price was: £7.81.£4.45Current price is: £4.45.
Product details
File Size: 2058 KB
Format: EPUB
Print Length: 150 pages
Word Wise: Not Enabled
Publisher: Addicus Books (1st November 2012)
Sold by: Books-For-Everyone Media
Language: English
Enhanced Typesetting: Enabled
ISBN: 1936374323
X-Ray: Enabled
Enhanced Typesetting: Enabled
Customer Reviews: ⭐⭐⭐⭐⭐ 2 customer reviews
Macular Degeneration: From Diagnosis to Treatment Kindle Edition
Macular Degeneration. With a focus on giving those diagnosed with macular degeneration the necessary information to make sound treatment choices, this reference aims to answer patients’ questions and ease their anxiety. The book provides information on the symptoms, causes, and emotional impact of macular degeneration; how the disease is diagnosed; choosing the right physician; and how to adapt the home and workplace to be “eye friendly.” In addition, it outlines the newest treatment options, drugs and surgical techniques, ways to slow the progression of the disease, and the importance of nutrition and general fitness on eye health. Written by two doctors with decades of experience treating thousands of patients, it supplies essential facts while affirming that people living with the disease can still enjoy a normal, happy life.
Product description
Review
About the Author
Home | Eye disease | What is macular pucker or epiretinal membrane?
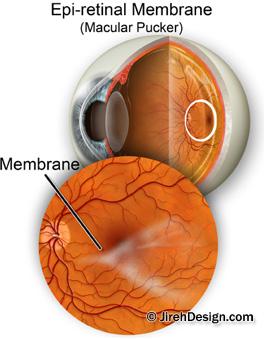
What is macular pucker or epiretinal membrane?
What is macular pucker? A guide to its causes, treatments and surgery options
Other Names for macular pucker: Epiretinal membrane, pre-retinal membrane, cellophane maculopathy, pre-macular fibrosis, retina wrinkle.
What is macular pucker?
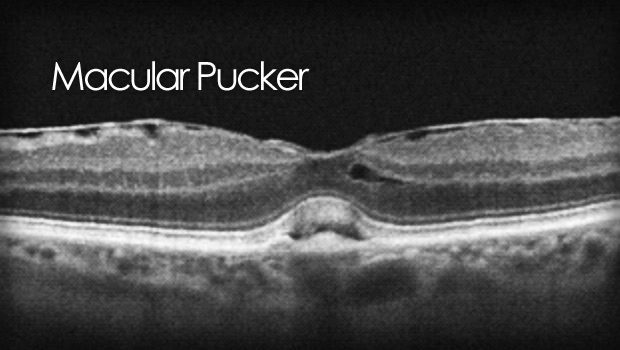
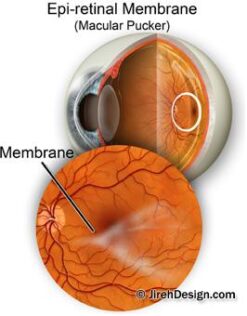
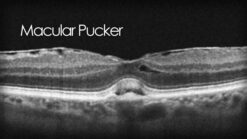
A macular pucker is scar tissue that has formed on the eye’s macula, located in the center of the eye’s light-sensitive tissue called the retina. The macula provides the sharp, central vision we need for reading, driving, and seeing fine detail. A macular pucker can cause blurred and distorted central vision.
Most of the eye’s interior is filled with vitreous, a gel-like substance that fills about 80 percent of the eye and helps it maintain a round shape. The vitreous contains millions of fine fibers that are attached to the surface of the retina. As we age, the vitreous slowly shrinks and pulls away from the retina’s surface. This is called a vitreous detachment, and is normal. In most cases, there are no adverse effects, except for a small increase in floaters, which are little “cobwebs” or specks that seem to float about in your field of vision.
Click here to watch a vitreous detachment movie
Sometimes when the vitreous pulls away from the retina, there is a small amount of damage to the retina’s surface. When this happens, the retina begins a healing process to the damaged area and forms scar tissue, or an epiretinal membrane, on the surface of the retina. This scar tissue is firmly attached to the retina’s surface. When the scar tissue contracts, it causes the retina to wrinkle, or pucker, usually without any effect on central vision. However, if the scar tissue forms over the macula, our sharp, central vision becomes blurry and distorted.
See a macular pucker surgery video here
What causes a macular pucker?
Most macular puckers are related to vitreous detachment, which usually occurs in people over age 50. As you age, you are at increased risk for macular pucker.
Certain eye diseases and disorders can trigger a macular pucker, such as a detached retina and inflammation of the eye (uveitis). Also, people with diabetes sometimes develop an eye disease called diabetic retinopathy, which can cause a macular pucker. Trauma from either surgery or an eye injury can also cause a macular pucker.
What are the symptoms of a macular pucker?
Vision loss from a macular pucker can vary from no loss to severe loss, although severe vision loss is uncommon. People with a macular pucker may notice that their vision is blurry or mildly distorted, and straight lines can appear wavy. They may have difficulty in seeing fine detail and reading small print. There may be a gray area in the center of your vision, or perhaps even a blind spot.
Is a macular pucker the same as age-related macular degeneration?
No. A macular pucker and age-related macular degeneration are two separate and distinct conditions, although the symptoms for each are similar. Your retinal specialist will know the difference.
Can macular pucker get worse?
For most people, visual acuity remains stable and does not get progressively worse. Usually macular pucker affects one eye, although it may affect the other eye later.
Is a macular pucker similar to a macular hole?
A macular pucker and a macular hole are different conditions, although they both result from the same reason: the pulling on the retina from a shrinking vitreous. When the “pulling” causes microscopic damage, the retina can heal itself; scar tissue, or a macular pucker, can be the result. If the shrinking vitreous pulls too hard, it can tear the retina, creating a macular hole, which is more serious. Both conditions have similar symptoms – distorted and blurred vision.
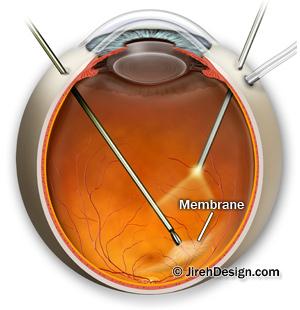
What is macular pucker surgery
A macular pucker sometimes requires no treatment. In many cases, the symptoms of vision distortion and blurriness are mild, and no treatment is necessary. People usually adjust to the mild visual distortion, since it does not affect activities of daily life, such as reading and driving. Eye drops, medications, and nutritional supplements will not improve vision problems caused by epiretinal membrane. Sometimes the scar tissue–which causes a macular pucker–separates from the retina, and the problem clears up.
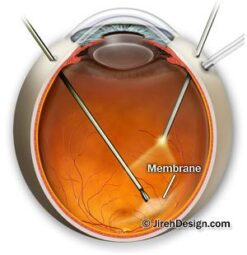
Sometimes, vision deteriorates to the point where it affects daily routine activities. When this happens, surgery may be the best option. This procedure is called a vitrectomy, in which the retinal surgeon removes the vitreous gel to prevent it from pulling on the retina and replaces it with a salt solution (because the vitreous is mostly water, you will notice no change between the salt solution and the normal vitreous). The surgeon also removes the scar tissue causing the wrinkling. A vitrectomy usually requires local anaesthesia. You can watch an animation of a vitrectomy surgery here.
After the operation, you will need to use medicated eye drops to protect against infection and swelling.
How successful is this surgery?
Surgery to repair a macular pucker is very delicate, and while vision improves in most cases, it does not always return to normal. Some people enjoy significantly more vision improvement, some less. In most cases, patients notice a significant improvement in vision distortion. Recovery of vision can take up to three months.
What are the risks of surgery?
The most common complication of a vitrectomy is an increase in the rate of cataract development. Cataract surgery may be necessary within a few years after the vitrectomy. Other less common complications are retinal detachment either during or after surgery, and infection after surgery. Also, the membrane may grow back, although this is rare.
Research
Research studies are being conducted to determine other treatments for macular pucker. Please note that both of the procedures described below need additional clinical testing.
Some physicians are researching the use of a surgical procedure in which scar tissue is peeled off without performing the vitrectomy.
Other doctors are researching a new surgical technique to remove the internal limiting membrane (a layer of the retina) for patients with both macular pucker and macular hole. This surgical technique is called Fluidic Internal Limiting Membrane Separation (FILMS). After a vitrectomy, the surgeon injects fluid between the membrane and the retina that allows the membrane, along with the scar tissue, to lift away. The surgeon then uses forceps to remove the membrane.
Watch a vitrectomy animation
See also…
ome information courtesy of the National Eye Institute
Tags: epiretinal, macula, macular, membrane peel, pucker, retina, surgery

Be the first to review “Macular Degeneration eBook” Cancel reply
You must be logged in to post a review.
Related products
Kindle Store
Non Fiction
Biography & Autobiography
Web Development
Marketing Books
Non Fiction
Non Fiction







Reviews
There are no reviews yet.